The pandemic was a critical time for health systems to step up and support the health and wellness of their communities. Like many health care providers, we saw a surge in patients seeking COVID testing and vaccination. While that was a huge milestone in stopping the spread of the deadly virus, we also saw a decline in patients scheduling their wellness visits and preventative screenings.
That decline forced us to begin reimagining our approach to patient care delivery. With the support of funding designed to support patients’ return to care from both the public and private sectors, ACCESS began to look at how to better engage our patients both within and beyond our health centers’ walls. From leveraging our electronic health record, Epic, to optimize communications between patients and providers to piloting culturally-focused, Spanish-speaking diabetes education support group at one of our largest health centers in Chicago, we are committed to finding new ways to engage our patients between visits to impact their overall health and quality of life.
According to SAMHSA’s National Survey on Drug Use and Health, only about 25% of U.S. adults received mental health treatment in 2023. With an increase in opioid use, anxiety, depression, and other mental illness disorders across our service area and the nation, we also believe that our model of care must continue to include expanded, integrated behavioral health services. From increased investment in our Medication Assisted Recovery (M.A.R.) program to add more sites and adding more psychiatry services, we understand the demand to have these resources all within one’s medical home.
Serving more than 160,000 patients each year across Chicago and in surrounding communities, we are more committed than ever to continuing to evolve our practices to better serve our mission and create a true medical home.
In Good Health,


Embedded within ACCESS’ mission is the responsibility to provide high-quality, patient-centered care, and we are always striving to build an organizational culture that supports this goal.
Since this work was launched in 2019, ACCESS has engaged staff in an organizational self-assessment and launched trauma-informed care pilot programs in select health centers. In 2022, in collaboration with the Patient Safety and Environment of Care and Trauma-informed Care StrategiCare Committees, ACCESS developed the 'Our Respectful Environment' statement, which is now installed in health center exam rooms and waiting areas. Additionally, ACCESS partnered with the National Council for Mental Wellbeing to develop the Trauma-informed Care 101 training program for staff, incorporating best practices and other key initiatives.
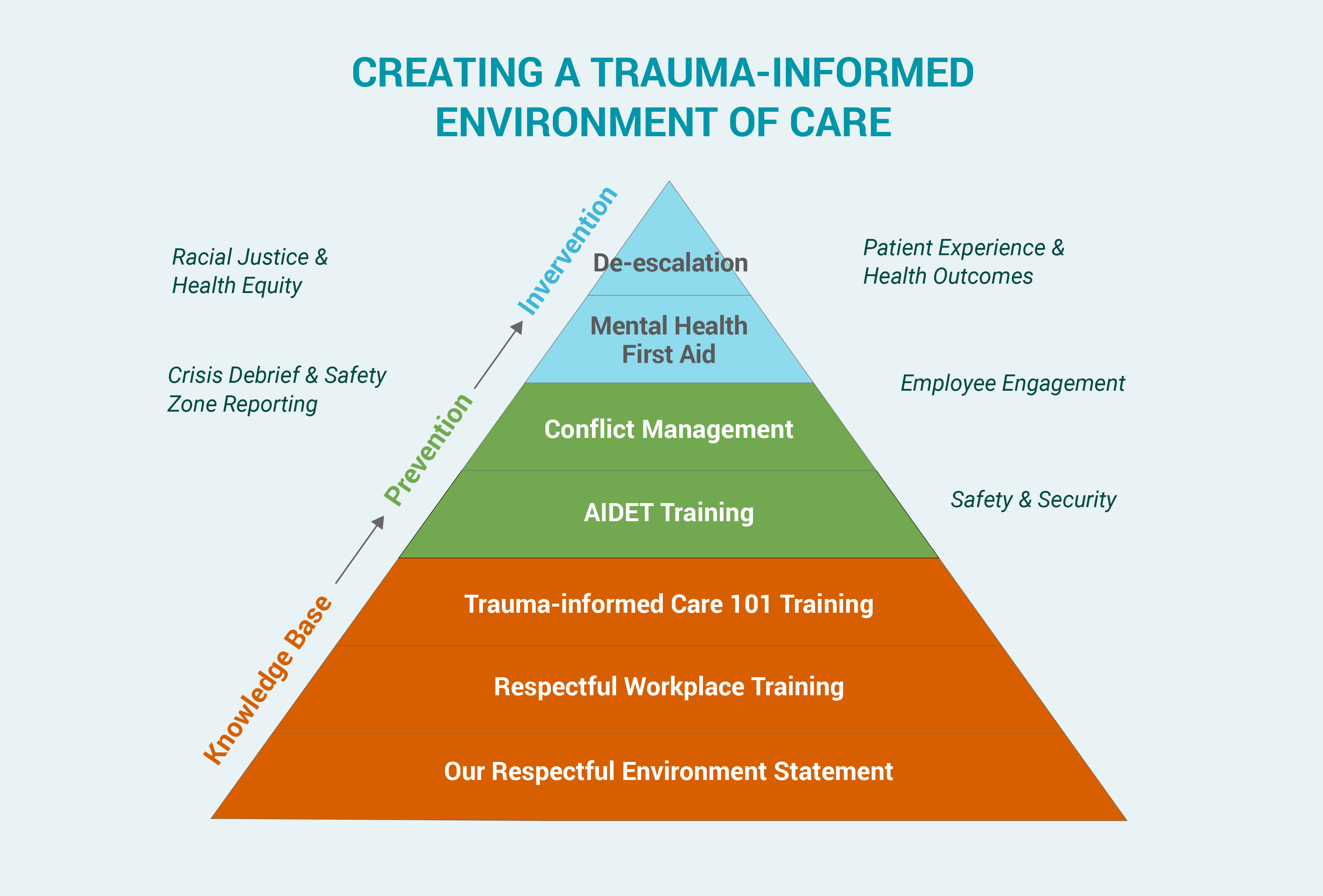
Trauma-informed Care acknowledges that understanding a patient’s life experiences is key to potentially improving engagement and outcomes while lowering unnecessary utilization. This approach is not limited to a clinical setting and can help us all in our interactions with family, friends, and colleagues.
Each year, ACCESS is taking measurable steps towards progress, and we are pleased to have an ongoing plan to complete AIDET® Plus the PromiseSM Communications Framework training for all health center staff.
AIDET stands for Acknowledge, Introduce, Duration, Explanation, Thank You and the Promise is our commitment to create the best experience, which could simply be letting a patient know that they can reach out with any other questions or restating that our staff are here to help improve patients’ health.
The acronym reminds health center staff of the five essential communication elements during interactions with patients or coworkers. It is not a script, nor does it need to be deployed in a specific order.
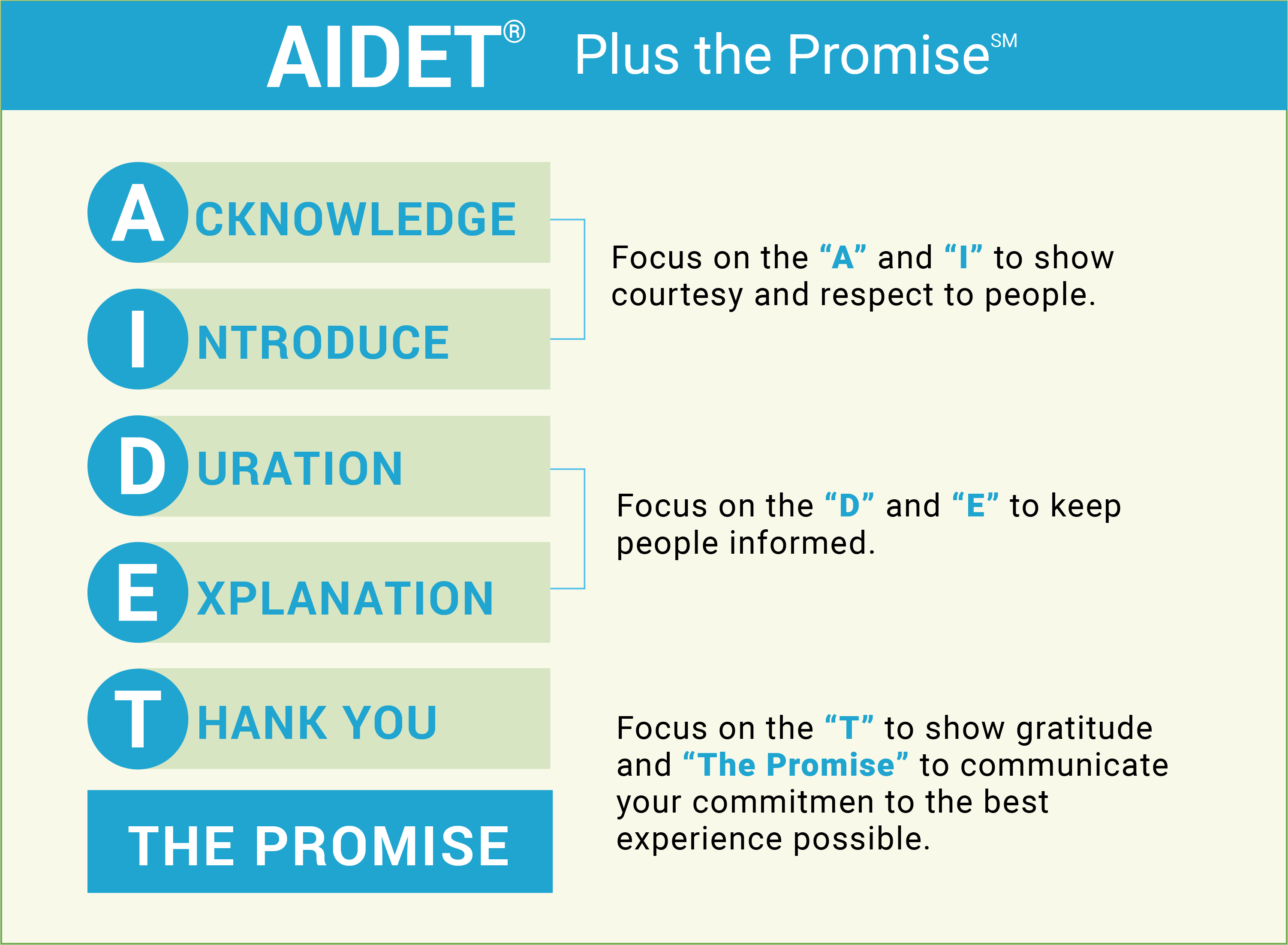
From scheduling an appointment through our contact center to checking in at the front desk, every interaction a patient has with ACCESS is important. The AIDET® Communications Framework enhances empathy and compassionate communication, reduces patient and coworker anxiety, fosters trust, improves collaboration and teamwork, and boosts patient and employee loyalty, while reducing patient complaints.

ACCESS is committed to an integrated model of care that reflects the needs of our patients and each individual community we serve. With an overall patient population that is 58% Hispanic, a bilingual approach to care that includes Spanish-speaking clinical care teams and culturally competent resources is essential in those communities, like Little Village, that are primarily Hispanic.
To address these disparities and meet the needs of our Spanish-speaking patients, ACCESS launched the Little Village Community Health and Wellness Program in Fall 2021 to provide bilingual nutrition education and support. Led by a registered dietitian with dedicated one-on-one sessions, patients participated in a six-week diabetes education course and/or a nutrition education course.
To learn first-hand the impact of our approach, ACCESS conducted a focus group with program participants. Among our findings, participants reported a change in diet, exercise, nutrition knowledge, diabetes maintenance, and health motivation. In fact, one participant Maya Diaz shared, “Now, what I really enjoyed about the class is the sense of community. Different people coming from different backgrounds come together to have this experience together. It feels better, knowing that other people were going through the same thing.”
According to the CDC, the Hispanic population experiences disproportionately higher rates of diabetes, hypertension, and obesity. While education about diet and nutrition is key to addressing these disparities, often the right resources are inaccessible or do not address the unique needs of communities of color.
Another key finding was the impact of integrating a bilingual and culturally competent diabetes educator. The dietitian was able to create tailored nutrition plans around the staple foods in Hispanic culture, including tortillas and beans, so that participants did not need to give them up completely, but were equipped with a better approach to practice portion control and meal planning.
By supporting participants in their nutrition goals, this program was also able to impact our patients’ families and improve the diets of the entire household. For example, patient Maria Sierra wanted a way to treat her diabetes through lifestyle changes and without medication. Through consultations with her ACCESS dietitian, she learned about how different foods impacted her blood sugar and found tips on how to cook family favorites just a little bit healthier. She shared those lessons with her diabetic husband and now they are both seeing improvements in their health.
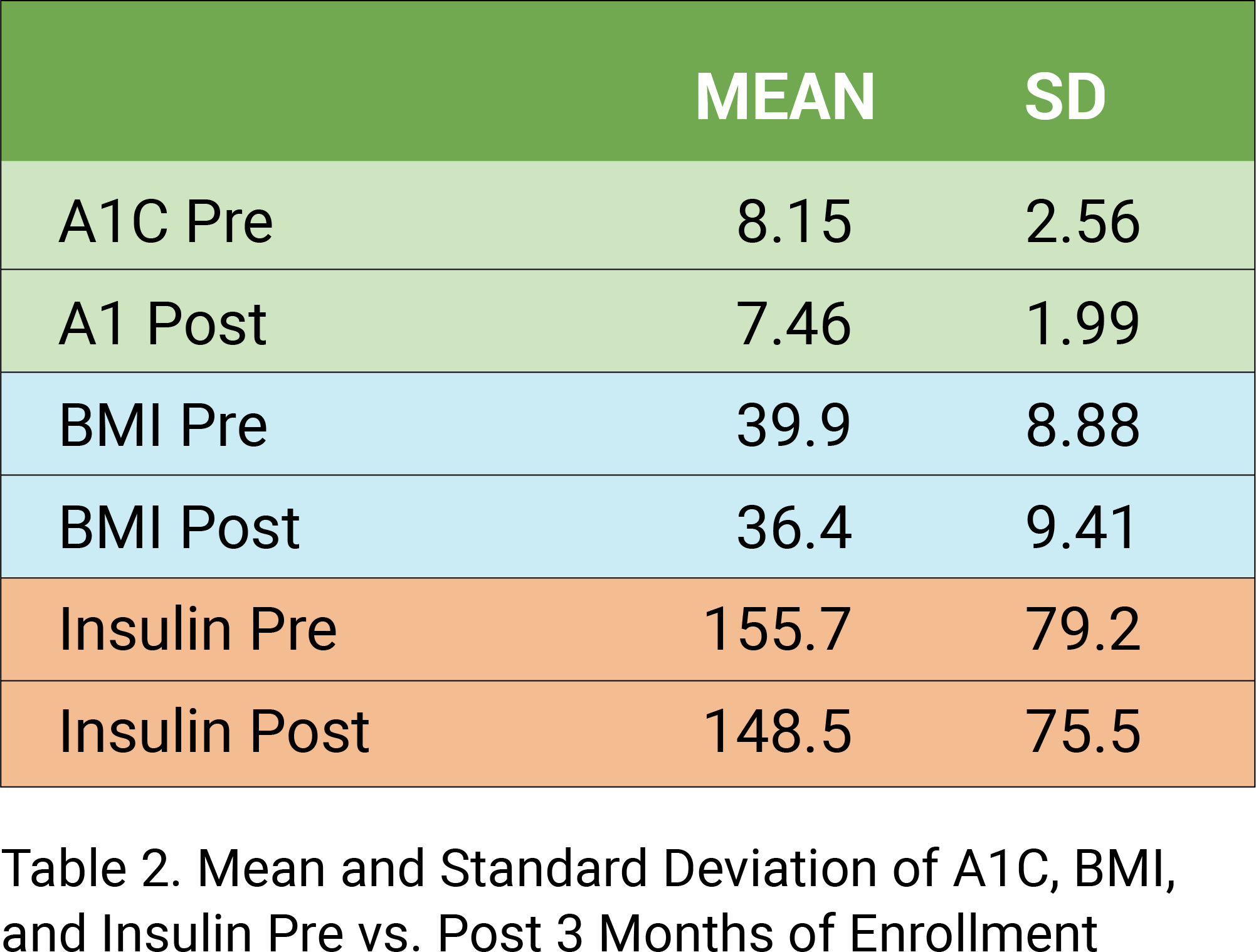
As shown in the data tables below, program participants overall experienced significantly improved A1C levels and moderately improved BMI numbers. Providing bilingual nutrition education in a culturally competent group and one-on-one format was an essential part of the success of the program. As ACCESS continues to evolve our model of care, we hope to create similar programs and will continue to invest in critical resources to support the overall health and wellness of our patients.


| 2023 | 2022 | 2021 | |
|---|---|---|---|
| Assets | |||
| Cash & Cash Equivalents | 33,078,492 | 39,505,866 | 35,172,888 |
| Patient Accounts Receivable, Net | 2,747,028 | 1,225,251 | 1,434,296 |
| Managed Care Receivables | 6,850,681 | 4,565,132 | 4,108,636 |
| Contracts and Grants Receivable | 2,612,359 | 2,792,710 | 4,498,893 |
| Other Receivables | 2,921,792 | 2,369,070 | 2,437,279 |
| Investments | 2,088,367 | 1,847,693 | 3,077,654 |
| Prepaid Expenses & Other Assets | 2,170,937 | 1,779,488 | 1,807,391 |
| Total Current Assets | 52,469,656 | 54,085,210 | 52,537,037 |
| Total Property & Equipment | 36,199,712 | 34,033,116 | 20,756,010 |
| 457(b) Plan Participant Assets | 3,435,940 | 2,816,332 | 3,169,024 |
| Right of Use Asset - Operating | 9,321,021 | 14,802,787 | — |
| Other Assets | 728,536 | 728,536 | 885,917 |
| Total Assets | 102,154,865 | 106,465,981 | 77,347,988 |
| Liabilities and Net Assets | |||
| Current Liabilities | 21,394,442 | 26,039,276 | 27,878,693 |
| Long-term Liabilities | 18,261,139 | 23,755,081 | 9,806,631 |
| Total Liabilities | 39,655,581 | 49,794,357 | 37,685,324 |
| Net Assets | |||
| Unrestricted | 61,802,179 | 55,858,215 | 38,761,983 |
| Temporarily Restricted | 697,105 | 813,409 | 900,681 |
| Total Net Assets | 62,499,284 | 56,671,624 | 39,662,664 |
| Total Liabilities | 102,154,865 | 106,465,981 | 77,347,988 |
RevenueOperating ExpensesOperating
|
|||
| 2023 | 2022 | 2021 | |
|---|---|---|---|
| Revenue & Other Support | |||
| Patient Service Revenue | 45,049,014 | 44,195,996 | 42,473,531 |
| Managed Care Revenue | 60,262,719 | 54,376,327 | 49,752,391 |
| 340B Pharmacy Revenue | 44,120,146 | 38,210,376 | 35,283,760 |
| Contributions & Grants | 33,938,172 | 42,132,459 | 31,012,135 |
| Other Revenue | 3,200,845 | 1,558,689 | 903,288 |
| Total Revenue & Other Support | 186,570,896 | 180,473,847 | 159,425,105 |
| Operating Expense by Function | |||
| Program Services | 142,655,828 | 138,308,526 | 124,923,009 |
| Management and General | 37,908,821 | 35,295,096 | 29,781,434 |
| Total Operating Expenses | 180,564,649 | 173,603,622 | 154,704,443 |
| Unrealized Gains on Investment | (62,283) | 226,007 | — |
| Gain on Debt Forgiveness | — | 10,000,000 | — |
| Change in Net Assets | 5,943,964 | 17,096,232 | 4,720,662 |

To assure quality and responsiveness to community health needs, more than half of Access Community Health Network’s Board of Directors are patients.
Thomas P. FitzGibbon, Jr.*
Kimi L. Ellen
Perla Herrera*
The asterisk (*) identifies patient representatives.

ACCESS provides a high quality, patient-centered care model using an integrated team-based approach, which engages patients across their lifespan at all points of care to best support the total health and well-being of the communities we serve.
ACCESS has an integrated network of partners with valued services and resources that help address the medical, behavioral, and social determinants of health that have the greatest impact on population health outcomes and total cost of care.
ACCESS is a resilient leader in navigating the ever-evolving health care landscape and creates diverse funding streams to invest in our infrastructure to expand services and support our transformation to a value-based reimbursement environment.
ACCESS has a strong team-driven culture that actively engages our diverse workforce at all levels while investing in learning and growth opportunities to provide the right tools and resources to care for our communities.
ACCESS is a champion for health equity, influencing public health policy, developing best practices, and adopting transformative approaches to drive innovative solutions to improve population health outcomes.